
views
A few months ago, All India Institute of Medical Sciences (AIIMS) blood bank in New Delhi received a desperate call requesting for a unique blood group. The call was made by the blood bank of Lady Hardinge Hospital where a Haryana-based woman in her late 20s had suffered a miscarriage and needed an urgent blood transfusion to remove the foetus.
Her haemoglobin was 6 grams per decilitre (g/dl) against the normal 12-15g/dl range. The call was received by Dr Hem Chandra Pandey, head, transfusion medicine (blood bank) at AIIMS, New Delhi.
“She was facing recurrent intra-uterine deaths. The blood group of the mother and unborn child was incompatible and in turn, the condition for the growth of the baby was difficult. Hence, she suffered the death of seven unborn children,” Pandey told News18.
“There are more than 400 blood groups that prevail across the globe and this woman had a group called D – – (dash dash) phenotype which is extremely rare.”
The AIIMS team checked the donor data in India but there was no donor available. The case was referred to AIIMS, and the doctors prepared for another emergency procedure to take the baby out while the mother’s haemoglobin was still low. “The team had no option but ended up removing the baby, successfully.”
Unfortunately, the woman had lost her seventh child too but she was saved despite acute anaemia. The team efforts reaped results when she came back to the hospital in her eighth pregnancy – again in a critical position. However, a team of over four doctors from the Department of Obstetrics and Gynaecology, including Dr K Aparna Sharma, Dr Vatsla Dadhwal, Dr Neena Malhotra, Dr Anubhuti Rana, and transfusion head Dr Hem Chandra Pandey, successfully saved her eight child and made history. The team performed a first-of-its-kind procedure in India and the eighth in the world.
Mission to Save the 8th Unborn Child
Dr K Aparna Sharma, from the Obstetrics and Gynaecology Department of AIIMS, told News18 that in this case, the incompatibility between the red blood cells of the mother and the baby in the womb led to problems for the unborn child due to the destruction of the red cells leading to anaemia, jaundice, heart failure and even death of the baby.
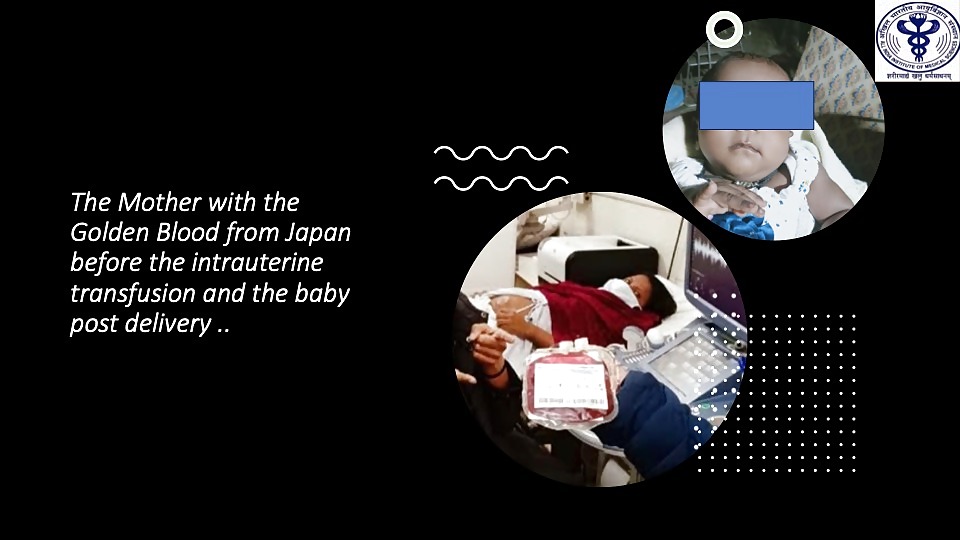
“The most common known incompatibility is due to the RhD antigen (commonly known as D+ or D-) and in severe cases of fetal anaemia RhD- blood is transfused to the baby inside the mother’s womb through the umbilical cord.”
However, in this case, Sharma said, the mother was negative for the Rh 17 antigen which is very rare to find. Due to this, the babies in her womb would suffer from incompatibility and develop anaemia and she had previous seven pregnancy losses.
“When she came to AIIMS in her seventh pregnancy, she had already lost her child inside her womb but in that pregnancy, the blood group was identified by the blood bank team. In her eighth pregnancy, she came to us during the fifth month and it was found that the baby was already anaemic and required blood to be given urgently.”
This time, the blood bank team moved aggressively as they had earlier sent the sample of the mother’s rare blood group to the United Kingdom’s International Blood Group Reference Laboratory.
The WHO-supported laboratory had sent the list of countries with donors of the same blood group.
“Now, was the time to use the list. We moved quickly as the list had given us names of around 10 countries. We zeroed in on Japan. The reason was simple – the country was relatively nearer and the list of donors was longer with almost 30 registered donors,” Pandey recalled. “We reached out to the Japanese Red Cross for around six units of blood that was planned to be given to the baby through the umbilical cord in the next few months to sustain the pregnancy.”
These specialised blood units were given as intrauterine transfusion and this procedure ensured the health and survival of an unborn child suffering from severe anaemia. The anaemia in child resulted from the destruction of red blood cells (hemolysis) caused by antibodies transferred from the mother. The condition is known as hemolytic disease of the fetus and newborn (HDFN).
The foetus received six blood transfusions inside the mother’s womb and the state of hydrops (heart failure) reverted to normal.
“The pregnancy continued till eight months when the baby was delivered by a caesarean section and this became the first case of a successful pregnancy outcome in a case of alloimmunisation due to Rh 17 Ag in India and eighth case in the world.”
According to studies, HDFN affects 3 out of every one lakh to 80 out of every one lakh patients every year. Haemolytic disease of the foetus and newborn is an immune-mediated red blood cell disorder. However, reasons and severity could vary from case to case.

















Comments
0 comment