views
Managing Non-Emergency Cases
Take an anticoagulant medication if your doctor prescribes one. If your doctor diagnoses you with a vein blockage that is not an immediate emergency, they may prescribe you a combination of medication and lifestyle changes, rather than more serious medical or surgical interventions. Often this includes being prescribed an anticoagulant medication, which will thin your blood and help prevent both the growth of your current vein-blocking blood clot and the emergence of new clots. Common anticoagulant medications include enoxaparin (Lovenox), warfarin (Coumadin), and heparin. They are very effective in many cases. Anticoagulants often require frequent blood tests to help fine-tune the dosage of medication you need. Since anticoagulants can cause complications, such as excessive bleeding, your doctor may not prescribe one of these medications if you have a low-risk clot (such as a clot below your knee that’s not causing any symptoms). Discuss the possible risks and benefits of using anticoagulants with your doctor.
Keep your blood flowing by moving around at least once per hour. Other than while sleeping at night, try not to sit, lie down, or even stand in place for more than 1 hour at a time. At least once per hour, take 2-5 minutes to get up, move around, stretch out, and do some light exercises. If you’re on the couch watching TV, get up and walk around or do light stretches during commercial breaks. If you’re at your desk at work, set a timer for every 60 minutes and do the same for 2-5 minutes. If you’re on a long plane flight, get up once an hour and move around the cabin to prevent clots. If you’re stuck in your seat for a long period of time due to turbulence, do seated exercises like rotating your ankles, lifting your knees, or alternating between raising your heels and toes. If you have vein blockages in your legs, your doctor may recommend a series of leg movements and stretches to do regularly—such as ankle rotations, pedal pumps, heel-toe rocks, knee-ups, and calf massages. Getting up and moving around regularly is good for your health whether you have blocked veins or not.
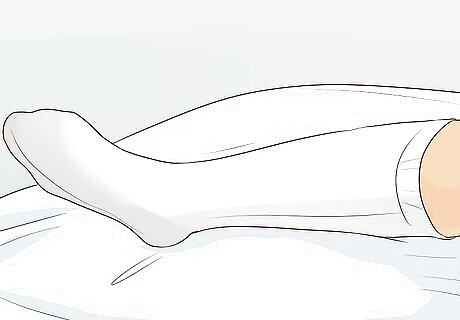
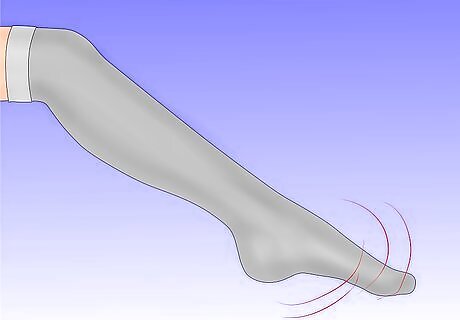
Wear compression stockings and elevate your feet for lower body blockages. Vein blockages can occur anywhere in the body, but your legs are one of the most common locations. If you have a lower body vein blockage—and possibly if your blockage is elsewhere—your doctor may tell you to wear prescription compression stockings and to keep your feet elevated while lying down. Compression stockings help to reduce the swelling that is commonly caused by blocked veins, and also help to prevent future blood clots in the area. You’ll probably be told to wear them during the daytime for a period of months or even years. Keeping your feet elevated as little as 1–2 in (2.5–5.1 cm) above your hips while sleeping or lying down may help reduce both the swelling and the likelihood of future clots. Try sticking a pillow under your feet while you sleep, for instance. Compression and elevation can also help with blockages in your upper body (such as in your arms). Ask your doctor to show you how to use compression sleeves, and keep the affected limb above your heart as much as possible.
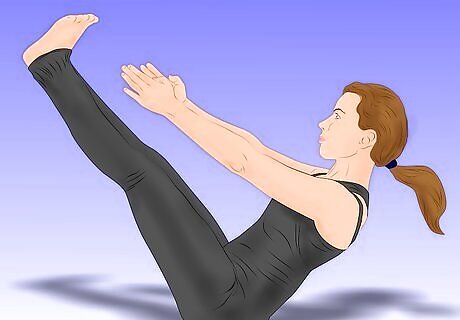
Follow a weekly cardio and strength training exercise regimen. The general recommendation for adults is to do at least 150 minutes of moderate intensity cardiovascular exercise per week, and to do 2-3 strength training sessions (lasting 30-60 minutes) per week. Your doctor will advise you whether you should have different weekly goals, based on your vein blockage and other health circumstances. “Moderate intensity” cardio means that you can still speak, but you’re breathing hard enough that it’s hard to carry on a conversation and impossible to sing a song. Fast walking, light jogging, and easy biking or swimming are usually considered moderate intensity cardio. Strength training can include free weights, machines, exercise bands, hand weights, or body weight exercises. Exercise improves your circulation, which helps stop the growth of any current blood clots and the development of new ones.

Stay adequately hydrated by drinking water throughout the day. Drink a full glass of water in the morning, before meals, and during meals, and take sips throughout the day before you feel thirsty.The amount of water you drink should be equal to half your body weight in ounces. Additionally, eat healthy foods with high water content, such as fresh fruits and vegetables. When your body is properly hydrated, your veins are better lubricated. This makes the growth of new or existing blockages less likely. Beverages other than water also provide hydration, but you should limit or eliminate your alcohol intake, as per your doctor’s orders. Alcohol can interfere with any anticoagulant medications you’re taking.
Eat foods that may help limit or prevent the growth of blood clots. Some foods have either proven or potential anticoagulant properties, while others have anti-inflammatory properties that may benefit your vein health. At the same time, some otherwise healthy foods, such as those rich in vitamin K, must be closely monitored if you’re on an anticoagulant medication. Consult with your doctor and a registered dietician to devise the best dietary plan for your situation. Common vein blockage-fighting foods include: omega-3-rich foods like salmon and walnuts; flavonoid-rich foods like dark chocolate; anti-inflammatories like garlic and turmeric; antioxidant-rich foods like grapefruit and pomegranate; and other foods such as grapes, cherries, cranberries, pineapple, kiwi fruit, apples, sweet potatoes, and beans. Foods like spinach, kale, and other dark leafy greens contain large amounts of vitamin K, which is essential to your blood’s ability to clot. Especially if you’re on an anticoagulant medication, it’s important for you to consume a consistent amount of vitamin K every day. Work with your doctor to plan your vitamin K intake.

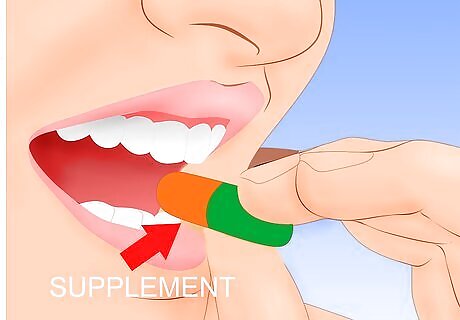
Take only doctor-approved vitamins and supplements. Some supplements and vitamins may help treat blocked veins, but others may interfere with your medications or cause other health problems. Tell your doctor about all the vitamins and supplements you currently take, and follow their advice regarding changes or additions you should make. You might, for instance, be advised to take a 500 mg omega-3 supplement 1-2 times per day. Omega-3 fatty acids have anticoagulant properties. You may be at an elevated risk for blood clots due to a high homocysteine level. Taking a prescribed daily dosage of vitamin B6, vitamin B12, and folic acid may help reduce your homocysteine level. Ginkgo biloba supplements may help thin your blood, but should only be taken with your doctor’s recommendation.

Treat serious and painful symptoms as an emergency situation. If you have been diagnosed with a non-emergency vein blockage and your symptoms worsen, get medical help right away. If you haven’t been diagnosed and experience serious symptoms, do the same. Vein-blocking blood clots can detach and lodge elsewhere in your body, potentially causing catastrophic or even fatal damage. Blood clots in the abdominal area can cause severe pain, vomiting, diarrhea, and bloody stools. Blood clots in the arms or legs can cause swelling, tenderness, and discoloration. Blood clots in the brain can cause speech and/or visual impairment, disorientation, dizziness, weakness or paralysis, and seizures. Blood clots in the heart can cause radiating chest pain, shortness of breath, an irregular heartbeat, and heavy sweating. Blood clots in the lungs can cause radiating chest pain, shortness of breath, a rapid pulse, and a bloody cough.
Treating Deep Vein Thrombosis

Seek immediate medical help if you have DVT symptoms. The type of vein blockage known as DVT is a serious medical issue that should be addressed right away. If you’re experiencing symptoms and can’t connect with your doctor immediately, go to your nearest hospital emergency department or call emergency services. Possible DVT symptoms include swelling (usually in just one limb), pain, and sometimes redness or discoloration of the skin near the clot. While DVT can occur anywhere, it’s most common in the legs. You’re at elevated risk of developing DVT if you are currently hospitalized, have recently had surgery, are elderly or immobile, are overweight or obese, have a family history of blood clots, have or have had cancer, are pregnant or have recently given birth, are taking hormonal birth control or hormone replacement medication, or have recently been injured. The blockage causing your DVT can break free and travel to your lungs, causing a potentially life-threatening pulmonary embolism (PE). Symptoms of PE include chest pain, shortness of breath, and coughing up blood. However, with prompt treatment, this is far less likely to happen.
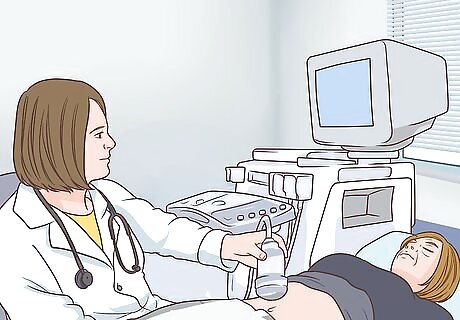
Undergo testing to properly diagnose DVT. To diagnose your DVT and determine its location, your medical care team will likely start by doing a simple, non-invasive ultrasound. If needed, they may then do additional diagnostic tests such as the following: Duplex ultrasonography, which is similar to a standard ultrasound but can more accurately track blood flow. D-dimer blood test, which checks a sample of your blood for clot fragments that have broken free. Contrast venography, which involves injecting a contrast dye into your bloodstream and then undergoing a series of X-rays.

Use IV, injection, or oral medications as prescribed by your care team. Depending on the location, severity, and other factors regarding your DVT, your medical care team will typically start treatment with one or more medications. These may include, but are not limited to, one or more of the following: Heparin. This is an anticoagulant that thins the blood and helps loosen the clot. It can be delivered by injection or IV and requires close monitoring afterward, which means you may have to stay in the hospital for 3-10 days. Low molecular weight heparin (LMWH). This option works similarly to traditional heparin but requires less rigorous monitoring. This means you may be able go back home instead of staying in the hospital. Warfarin. This is an anticoagulant that comes in pill form and works more slowly and less aggressively than heparin. You may be prescribed a daily warfarin dose for days, weeks, or permanently, and you’ll need to have blood testing done as often as 2-3 times per week while on warfarin. “Clotbusters” like TPA. Unlike anticoagulants, clotbusters actively work to break up a blood clot. They are delivered by IV, are reserved for the most serious cases, and require close monitoring in the hospital.
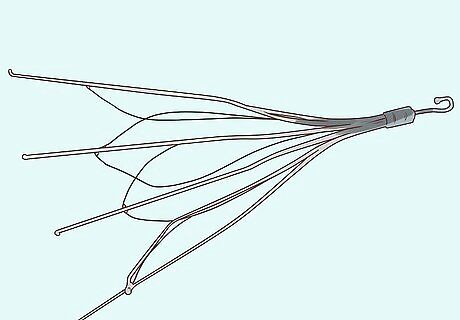
Have a vein filter surgically installed when medications aren’t viable. If you can’t use anticoagulants due to other medical factors, if the drugs are ineffective, or if your DVT is severe and calls for surgical intervention, you may need to have a vein filter surgically inserted into the inferior vena cava, the large vein that carries blood to your heart from your lower body. This can help prevent clots from traveling from your legs into your lungs. While this sounds extremely invasive, it can actually be done with a catheter passed through a small incision in your groin or neck while you’re awake. The filter itself is basically a soft mesh device that lets blood pass through but prevents the clot from passing by and potentially lodging in your lungs. You may need to have the filter in place for an extended period of time or very briefly, depending on your condition. However, these filters usually aren’t left in place permanently. Once your doctor thinks it’s safe to remove the filter, they will take it out basically the same way they put it in, through a catheter in your neck. It’s rare for these filters to cause any pain or discomfort. You probably won’t even be able to tell that it’s in there doing its job!
Make dietary, activity, and lifestyle changes as advised by your care team. As part of your treatment for DVT, your medical team will likely prescribe a range of adjustments. These changes are similar to those advised for anyone with a blocked vein due to a blood clot, including non-emergency cases. You’ll further improve your already-good odds of a successful recovery by taking simple measures like the following: Moving around at least once per hour and elevating your feet at night. Wearing compression stockings during the day. Following a weekly cardio and strength training exercise program. Staying hydrated by drinking water. Eating foods and taking vitamins and supplements that may help prevent the growth of blood clots.
















Comments
0 comment