views
X
Research source
If you are unsure if a baby is affected by these or any other symptoms and you think that something is not right, head to the emergency room immediately.
Checking Your Baby for Signs

Look for early symptoms. The earliest symptoms of meningitis include vomiting, fever, and headaches. With babies, there are different ways to detect the signs and symptoms of meningitis since the baby cannot communicate their pain and discomfort to you with words. Symptoms can progress quickly between 3 to 5 days of initial infection. It is therefore important to get your baby to medical attention immediately.

Examine your baby's head. Examine and lightly feel all around the baby's head for bulging and tense soft spots. The bulging soft spots will most likely appear on the sides of the baby's head in their fontanelle regions, which are gaps present in the baby's skull as their cranium continues to develop., A bulging fontanelle is not always indicative of meningitis. Regardless of the possible causes, a bulging fontanelle is always an emergency and you must take your baby to an emergency room immediately. Some other conditions that cause a bulging fontanelle include: Encephalitis, which is swelling of the brain, usually caused by an infection. Hydrocephalus, caused by fluid buildup in the brain. This can happen because of an obstruction or narrowing of ventricles that help channel fluid out. Increased intracranial pressure, caused by a build-up of fluid. This can restrict blood flow to the brain.
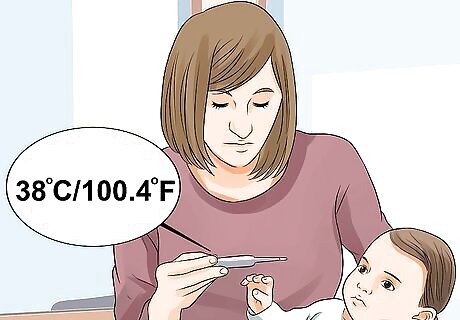
Take your baby's temperature. Use an oral or rectal thermometer to check for fever. The baby may have a fever if the temperature is above 37.5ºC (99.5ºF). A very high temperature could be a sign of a medical emergency, depending on the baby's age: Under 3 months of age, always seek medical attention for a temperature above 38°C (100.4°F). 3–6 months: always seek attention for a fever above 39ºC (102.2ºF). Older than 6 months: always seek attention for a fever above 40°C (104°F). Do not rely solely on a high temperature to tell you that you should take the baby to an emergency room. Babies younger than three months with meningitis often have no fever.

Listen to how the baby cries. If your baby is ill, she will display irritability such as crying, moaning or thrashing. This may happen especially when you pick her up due to painful, achy muscles and joints. She may be quiet when she is stationary, but she will start crying loudly when picked up. Listen for changes in the baby's crying that may indicate pain or discomfort. The baby may whimper and moan excessively or emit cries that are higher than normal in pitch. The baby might also have pained or extreme crying when you cradle her or touch the neck area. Bright light might also trigger crying due to photophobia.

Watch for signs of stiffness in the baby's body. If you suspect meningitis, examine and watch the baby for signs of stiffness in her body, especially in her neck. The baby may not be able to touch her chest with her chin, and she may display jerky, abrupt movements.

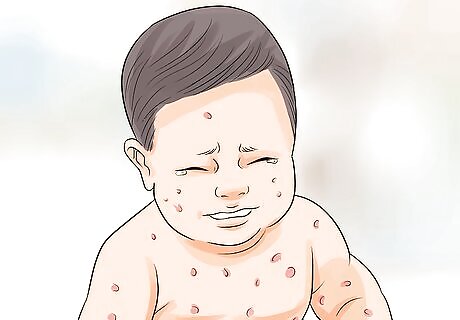
Examine the baby's skin for discoloration and rashes. Take a look at the baby's skin tone and complexion. You may observe skin that is extremely pale or blotchy, or it might have developed a bluish hue. Look for rashes that are pink, purple-red, or brown or develop rash clusters of pin-prick dots that resemble bruises. If you are unsure whether the blotchy spots on the baby is a rash, you can verify by using the tumbler/glass test. This is done by gently pressing a clear drinking glass to the affected area of the skin. If the rash or red spots do not disappear because of the glass being pressed against the skin, the baby most likely has a rash. If you can see a rash through the clear glass, go to the emergency room immediately. If the baby has a darker complexion, a rash may be difficult to observe. In this case, look at areas such as the palms of the hands, the soles of the feet, the stomach, or near the eyelids. These areas may also have what resembles red dots or pinpricks.

Take note of the baby's appetite. Your baby may not appear as hungry as usual. She may refuse to eat when you try to feed them and vomit anything they ingest.

Examine the baby's energy and activity levels. Look for signs of weakness. The baby may appear limp, lifeless, and tired or may appear sleepy constantly regardless of the rest they have received. This occurs as the infection spreads throughout the meninges.

Listen to the baby's breathing patterns. Observe the baby for irregular breathing patterns. The baby may breathe faster than normal or have difficulty breathing.

Feel the baby's body for coldness. Observe if the baby seems to have extreme, constant shivering and unusual coldness, especially on her hands and feet.
Know what meningitis is. Meningitis occurs when an infection causes the meninges or the tissue that lines your brain and spinal cord to become inflamed and swollen. The infection is usually due to certain bacterial or viral invasion into the baby's system. Causes of meningitis include: Viral: This is the number one cause of meningitis in the world, and it may resolve on its own. However, the baby still needs to be seen by a medical professional because the effects of the infection can be deadly if supportive care isn't provided. For children and babies, it is important for the parent or guardian to follow all immunization protocols. Mothers who are infected with herpes simplex virus or HSV-2 can transmit the virus to their baby during labor, if the mother has active genital lesions., Bacterial: This type is common in newborns and babies. Fungal: This type of meningitis is uncommon and usually affects AIDS patients as well as others who have compromised immune systems (e.g. transplant recipients and patients receiving chemotherapy). Miscellaneous: Other types of meningitis may be chemical, drug, inflammatory and cancer.
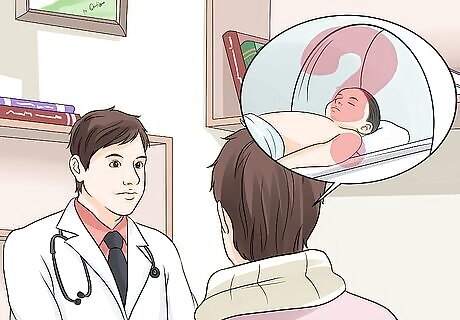
Getting a Diagnosis from a Doctor

Tell the doctor about all symptoms. Describe all symptoms to your doctor, including ones that seem minor like sneezing or coughing. This will help your doctor distinguish between different types of meningitis, and move on to the appropriate diagnostic test. Tell the doctor about these severe symptoms immediately, as they may require emergency treatment: Seizures Loss of consciousness Muscle weakness

Tell your doctor if your baby has been exposed to certain bacteria. There are several strains of bacteria that cause meningitis. If your baby has been exposed to people with a stomach illness or respiratory illness, he or she may have been exposed to any of these categories of bacteria: Strep B: In this category, the most common bacteria causing meningitis in babies under 24 months is strep agalactiae. E Coli Listeria species Neisseria Meningitidis S. Pneumoniae Haemophilus Influenzae

Have your baby get a complete physical examination. The doctor will take your baby's vitals as well as her medical history. The doctor will take the baby's temperature, blood pressure, heart rate, and respiratory rate.
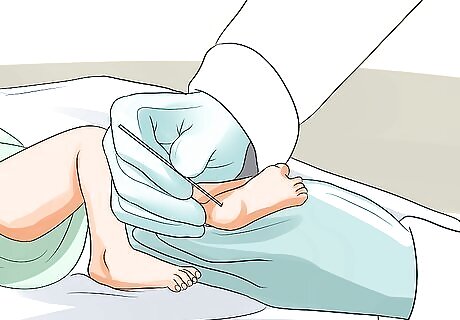
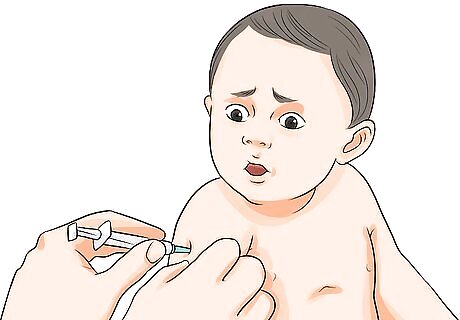
Let the doctor draw blood. The doctor will draw blood from the baby in order to do a complete blood count. The doctor will take blood by poking a small hole in the baby's heel. The complete blood count will examine electrolyte levels, as well as red and white blood cell counts. The doctor will also check blood coagulation and will check for bacteria in the blood.
Ask the doctor about a cranial CT scan. A cranial CT scan is a radiological test that checks the density of the brain to see if soft tissues are swollen or if any hemorrhaging has occurred. If patient has had a seizure or any trauma, a CT can help find this as well as indicate whether the patient can have the next test which is a lumbar puncture. If the patient has any indication of high intracranial pressure due to any of the previously mentioned indications, a lumbar puncture will not be initiated until pressure has decreased.
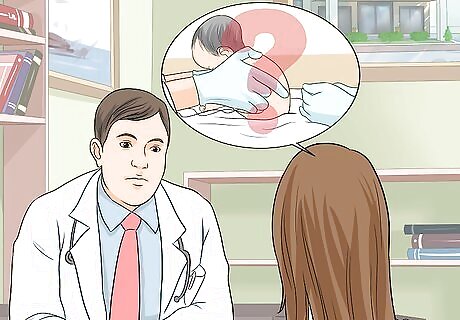
Ask if a lumbar puncture is necessary. This test extracts cerebrospinal fluid from the baby's lower back. The fluid is needed to administer certain tests in order to determine the cause of the meningitis. Be warned that this test is painful. The doctor will apply a topical anesthetic and use a large needle to pull fluid out between the bones of the patient's lower back. If certain conditions are present, the doctor will not perform a lumbar puncture. These conditions may include: Increased intracranial pressure or cerebral herniation (cerebral tissue shifting from its normal location) Infection at the site of lumbar puncture Coma Abnormalities of the spine Difficulty breathing If the lumbar puncture is necessary, the doctor will use the cerebrospinal fluid to administer tests, which may include: Gram stain: Once cerebrospinal fluid is removed, some of it will be stained with a dye in order to determine the type of bacteria present in the fluid. Cerebrospinal fluid analysis: This test analyzes the fluid sample for cells, protein and glucose-to-blood ratio. This can help doctor correctly diagnose meningitis and differentiate each type of meningitis from one another.
Getting Treatment for Meningitis

Get your baby treated for viral meningitis. Meningitis is treated based on the type. Viral meningitis is treated depending on the viral cause. For example, HSV-1 or herpes may be transmitted from mother to baby during labor if the mother has active genital lesions. Treatment for a newborn diagnosed with herpes encephalitis should be treated with an intravenous antiviral agent (for example, acyclovir administered intravenously).

Follow the treatment plan for bacterial meningitis. Bacterial meningitis is also treated based on the bacterial cause. Your doctor will identify this cause and give your child the appropriate treatment. Follow your doctor's instructions for administering the treatment. Below are some suggested medications and dosages: Amikacin: 15-22.5 mg/kg/day every 8-12 hours Ampicillin: 200-400 mg/kg/day every 6 hours Cefotaxime: 200 mg/kg/day every 6 hours Ceftriaxone: 100 mg/kg/day every 12 hours Chloramphenicol: 75-100 mg/kg/day every 6 hours Co-trimoxazole: 15 mg/kg/day every 8 hours Gentamicin: 7.5 mg/kg/day every 8 hours Nafcillin: 150-200 mg/kg/day every 4-6 hours Penicillin G: 300,000-400,000 U/kg/day every 6 hours Vancomycin: 45-60 mg/kg/day every 6 hours
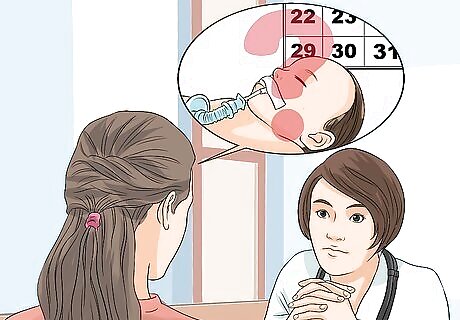
Talk to the doctor about how long the treatment will last. The duration of treatment for your baby's meningitis depends on cause of meningitis. These are some estimated lengths of treatment: N meningitides: 7 days H. Influenza: 7 days Strep pneumonia: 10 to 14 days Group B. Strep: 14 to 21 days Gram negative aerobic bacillus: 14 to 21 days Listeria monocytogenes/L. meningitis: 21 days or more

Give the baby additional supportive care. Give your baby care to ensure that she receives her proper dosages of medication throughout the entire course of treatment. She should also be encouraged to rest and consume lots of fluids. It is likely that an IV fluid will be provided due to her young age. She should also be prevented from transmitting meningitis to other family members.
Following Up After the Meningitis Treatment

Get your baby's hearing evaluated. Hearing loss is the most common complication of meningitis. Therefore, all babies must have hearing evaluated post treatment through auditory evoked potentials studies.
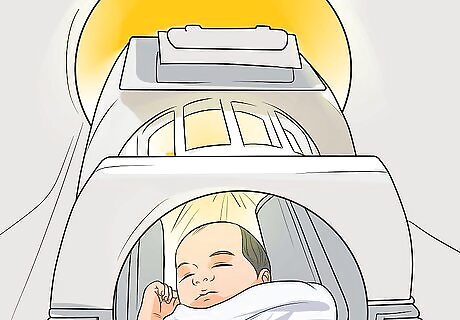
Check your baby's intracranial pressure with an MRI. Post-treatment bacteria or other pathogens can remain and cause complications. One of these is increased intracranial pressure from a build-up of fluid between different compartments of the brain. All babies must undergo a follow up MRI 7 to 10 days after treatment for meningitis has ended.
Vaccinate your child. Be sure your child has had all vaccinations in order to reduce the chance of getting viral meningitis. Reduce the risk of future children getting meningitis. If you are pregnant and you have HSV with genital lesions present, inform your doctor before delivery.
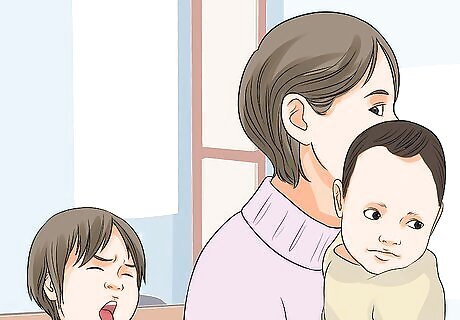
Eliminate contact with contagious or sick individuals. Some forms of bacterial meningitis are contagious. Keep young children and babies away from contact with contagious or sick individuals.

Be aware of risk factors. Some people may be at higher risk for contracting meningitis, depending on certain circumstances. Some of these include: Age: Children under five years old may be at higher risk for viral meningitis. Adults over the age of 20 may be at higher risk for bacterial meningitis. Living in close quarters: When people live in close contact with many other people, such as dormitories, military bases, boarding schools and child care facilities, they may be at increased risk of meningitis. Decreased immune system: People with compromised immune systems may have a higher risk of contracting meningitis. AIDS, alcoholism, diabetes, and use of immunosuppressant drugs can compromise immune systems.
















Comments
0 comment